
Understanding Risk Reduction vs Prevention: Why it Matters to Your Mental and Physical Well-Being
What you’ll learn in this article:
- It’s important not to blame yourself for developing preeclampsia: there’s currently no absolute way to prevent it from happening.
- “Risk reduction” doesn’t equal “disease prevention.”
- You can do some things that could lower your risk of getting preeclampsia, but there’s still no guarantee you won’t get it.
As a preeclampsia or HELLP syndrome survivor, you may struggle as you try to make sense of what happened: Why me? Could I have done anything to prevent it?
It's normal to feel that way, but rest assured: You are not in any way to blame for what happened. As expectant mothers, we’re so focused on our baby’s well-being that when preeclampsia strikes, we tend to blame ourselves. Sometimes that blame can also be imposed by well-meaning, but ultimately frustrating, loved ones or care providers.
Survivors frequently contact us to ask:
- “I exercised, ate right, and went to all my doctor’s appointments. How could I have gotten preeclampsia?”
- “Did I do something that caused me to get preeclampsia?”
- “How do I explain to my family and friends what happened to me so they understand there was no way I could have prevented this?”
It’s very easy to confuse the idea that you somehow “caused” your preeclampsia with the understanding that there are some individual health risks for developing preeclampsia you can control.
We don’t yet completely understand what causes preeclampsia, so there’s currently no way for you to absolutely prevent getting it. But we do understand some of the risk factors for developing it, so there are things you can do to reduce your risk. Understanding the difference between “disease prevention” and “risk reduction” is crucial.
Disease prevention = being at 0 on the chance scale, where it’s impossible for you to get that disease
Disease risk reduction = sliding your individual risk factors away from “certain”, but without definitively reaching “impossible”
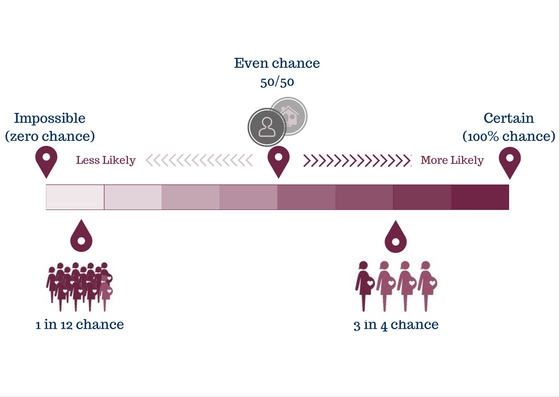
For an everyday example, consider hand-washing. While washing your hands helps reduce your risk of getting sick, it doesn't ensure you'll never get sick. If there are things you can to do move your chance of getting preeclampsia from the 3-in-4 chance end of the scale closer to the 50/50-even chance, or even the low "1 in 12" risk enjoyed by the general population, it’s a good idea to do it.
There's no evidence, however, that you can do anything to move your personal risk to the zero (“impossible”) end of the scale.
Understanding general risk versus individual risk
Individual health risk factors are all the situations that make someone more or less likely to develop a disease. When we think about factors that influence our risk of getting preeclampsia, many of those factors are things that are completely out of our control, like being a first-time mom, genetics, or family history. Others factors are more or less controllable, like weight or how well controlled our blood pressure is going into our pregnancy.
General population risk is the chance of something happening within a set group of people. For example, some research suggests that the general risk of developing preeclampsia in the U.S. may be as high as one in 12 pregnancies; other studies say it is much lower – like one in 25.
Each patient goes into her pregnancy with a specific individual health risk (or likelihood) of developing preeclampsia. That risk may be more or less than that of the general population.
Accepting, but minimizing risk: “Why we put on our seatbelts”
Accepting risk is something we do every day of our lives. For example, getting into a car and driving to the grocery store is a calculated risk: you might get in a fatal accident along the way. Thankfully, the general population risk of getting into a fatal crash is fairly low, but it still occasionally happens.
Strong, evidence-based research has shown that wearing a seatbelt greatly reduces your risk of dying because of a car accident. Wearing a seatbelt won’t prevent you from getting into a car accident. It may, however, save your life.
So we accept our risk of a fatal car accident by driving every day... but we also wear our seatbelts.
So too it is with preeclampsia. There are things we can do to reduce our risk. When possible, we should address those things.
Some preeclampsia risk-reduction interventions are being added to continuing care recommendations, such as taking low-dose aspirin. Low-dose aspirin doesn’t prevent preeclampsia for all individual patients, but it has been shown – through several research studies and combining their results into a “meta-analysis” – to lower that general population risk. That's why it's being widely recommended for women at high risk for preeclampsia.
The same can be said for controlling your blood pressure or diabetes, or trying to start your pregnancy at a healthy weight. We know that unchecked high blood pressure, diabetes, or being overweight increases your risk of developing preeclampsia. Not improving these controllable risk factors doesn’t mean you caused your preeclampsia, any more than not wearing a seat belt caused your car accident. It does, however, serve our best interests to do everything possible to reduce the chances of something bad happening by addressing any of the “modifiable” risk factors that may apply to you through evidence-based risk reduction activities.
That’s where self-responsibility and self-blame sometimes get improperly mixed together.
Putting self-care at the heart of your recovery process
It's important to remember that you might have controlled all these modifiable risk factors, but still developed preeclampsia or HELLP syndrome. It happens to many other women just like you.
You might find yourself playing a “what if” game after your preeclamptic pregnancy. Recognize that “what ifs” rarely result in productive answers.
Be kind to yourself. (And don’t let others be mean either!) If you’re still in the immediate throes of anger and grief over your experience, it can truly help to reassure yourself that there was no way you could have prevented what happened to you. (Besides not getting pregnant, which may not have been a desired option!)
Once you’ve put some distance between you and your preeclamptic pregnancy, something good can come from your “what if” statements, such as asking, “What if my healthcare provider included preeclampsia symptoms education during my prenatal visits?”
Perhaps your answer provides the fire you need to advocate for your doctor’s office, local hospital, or even entire state to take up the new standard of care that includes patient education for every woman, every pregnancy. Perhaps your answer encourages you to volunteer for your local Promise Walk for Preeclampsia and provide support to local families.
Knowing all this may help ease your mind about what happened to you. But if you still find yourself overwhelmed, know that you’re not alone: Many women who survive preeclampsia find the experience to be overwhelming, and for that reason, we encourage you to seek out counseling or other services to help you cope.
For more tips on dealing with the emotional burdens of preeclampsia and HELLP syndrome, visit these additional links:
Not Just Physical: The Psychological Burden of Preeclampsia and HELLP Syndrome
Picking Up the Pieces: Emotional Recovery Following Preeclampsia and HELLP Syndrome
A special thanks to Joy Victory and Heather Alonge of our Patient Advisory Council and Dr. Tom Easterling of our Medical Advisory Board for their review of this article.
Original article written January 2017; updated November 2020.
Related Articles

Doulas can help bridge the gap for any mom, but especially those most vulnerable to maternal illness and death.

Stories of our brave women and families who have been affected by preeclampsia and HELLP syndrome. Please note that due to a technical issue, we are currently fixing the images on this page.

What is Preeclampsia? Preeclampsia is a hypertensive disorder that occurs only during pregnancy and the postpartum period and affects both the mother and the unborn baby. Affecting at least...

Birth Trauma Resources Between 25 and 34 percent of women report that their births were traumatic. A traumatic birth experience is defined by circumstances in which the individual patient bel...

How does preeclampsia affect health after pregnancy? Preeclampsia doesn’t always end with delivery. It is now recognized as an early warning sign for future cardiovascular disease. Women who h...

Shattered Expectations: What happens after the unexpected? You may have received the unexpected news that you have preeclampsia or another hypertensive disorder of pregnancy. Maybe labor complic...

Even after more than twenty years, Mavis “Mae” Stephens, a 3x preeclampsia survivor, vividly remembers the challenges she faced during her pregnancy with her second son. She did everything...

Recientemente, me encontré con una publicación en las redes sociales señalando la crisis de salud maternal desde la perspectiva de una mujer negra. Una persona respondió a...

Meghan Markle is opening up about her experience with postpartum preeclampsia in the debut episode of her new podcast, Confessions of a Female Founder. In the episode with her first guest and clo...

