
Nurses Matter - 10 Ways You Support Patients
This article was originally written in 2013, but is still especially relevant today on National Nurses Day during the COVID-19 pandemic. Thank you to all the many nurses and midwives in our community who do what is best for their patients!
In 2013, a nurse from the University of Illinois Medical Center asked the Preeclampsia Foundation, "What do you think we, as nurses, could do to support patients when they are in a situation (preeclamptic pregnancy) similar to yours?"
We wondered aloud and nearly three dozen survivors responded via Facebook and our online Community Forum to share their experiences and provide their suggestions to the nursing profession. While there was very vocal appreciation for the majority of nurses who have cared for our women, there were also many helpful suggestions. Based on patient input, here are...
Top 10 Ways Nurses Support Preeclampsia Patients

1. Knowing the symptoms, educate your patients. Know how dangerous preeclampsia can be, know the full breadth of possible symptoms, and be proactive about diagnosing and managing it. The Foundation's motto "Know the Symptoms, Trust Yourself" is targeted at pregnant women, but as healthcare providers, you can help those of us who may not know the signs and symptoms.
2. Being willing to listen and learn. We know your shifts are busy and your demands are many, but listen to us, your patients. Don't ignore symptoms we report. Be willing to be educated and educate us also. Tell us about the Preeclampsia Foundation so we can get additional support and more information.
3. Avoiding falling victim to common medical errors. Medical acuity is always important in the hospital setting. With a syndrome as complex as preeclampsia, the details definitely matter! Common medical errors such as taking BP in the wrong position, retaking it until you find a pressure you "like", or not staying on top of delayed test results, can add stress to our already traumatic experience. (Read our Top 10 Preeclampsia Myths article here!)
4. Being sensitive to vulnerable emotional states. Don't hold it against us or inadvertently make it worse. With or without perinatal loss, there is often great emotional strain on the patient and family; different family members may be feeling different emotions from one another (e.g., fear, sadness, anger, relief, emptiness, joy) or be focusing on conflicting factors (i.e., mom vs. baby). We do appreciate the care you are giving to us, but may not be in the best frame of mind to make that clear to you.
5. Showering us with compassion and kindness. Even though some patients may drive you nuts with their demands and "high maintenance", survivors of complicated pregnancies have additional physical and emotional traumas, are often in severe pain, and are usually shocked by any bad outcomes during childbirth. Please show us extra compassion and be patient with our needs. Your actions will be forever remembered. Remember that magnesium sulfate makes us feel horrible! "I think it was the little things that I appreciated, like helping change my daughter's diaper or helping me with her first bath. That is stuff we really want to be a part of when we are feeling better and strong enough." "One nurse in the ICU washed and braided my hair for me - it was a small gesture, but it did make me feel a lot better."
6. Being aware of post traumatic stress disorder (PTSD) risks inherent in complicated pregnancies. Even without longer term PTSD, there will likely be short-term emotional pain, beyond post partum depression. And the dads are not immune, although they may look stronger in the short term. Even without a formal screening process, nurses can play an important first line of defense to help us be aware of the impact preeclampsia may be having.
7. Being aware of the impact that your shift and location changes can have on patients. As with any hospital patient care, there are almost always opportunities to improve team communication among healthcare providers, especially during shift changes, to ensure standards of care are upheld. In addition, if we're transferred post-partum to another ward, the original labor and delivery nurses can play an important role in the transition by sharing sensitive emotional care information to other staff.
8. Being honest with us. Tell the truth . . . but with compassion, friendliness, and caring. Don't tell us not to worry, but tell us what we should be looking out for. We rely on you because you are the expert on our medical care.
9. Helping patients and their families cope with a loss or having a baby in the neonatal intensive care unit (NICU). Nurses can devise a way to alert visitors and all health care staff that there has been a loss (e.g, hang a small wreath on the door) or that baby is in the NICU, preventing inappropriate comments and questions. Similarly, please be sensitive to what we may overhear from nearby happy-outcome families. "I was put on the ward with women who had delivered healthy living babies...that was the worst experience of my life. I thought I would die just from the emotional pain."
10. Remembering that your patients may be struggling with feelings of guilt for having failed at pregnancy. Nurses may directly or inadvertently contribute to this misplaced guilt by suggesting that we could have eaten more/less/different foods, exercised more/less, weighed more/less, etc. "Bugging me over the should/would/could haves will only make things more painful!" Remember that high blood pressure is called "the silent killer" for a reason. Many patients are unaware of their rising blood pressure until they are checked by you, our nurses. Thank you to those nurses who remind us that it is not our fault!
Related Articles
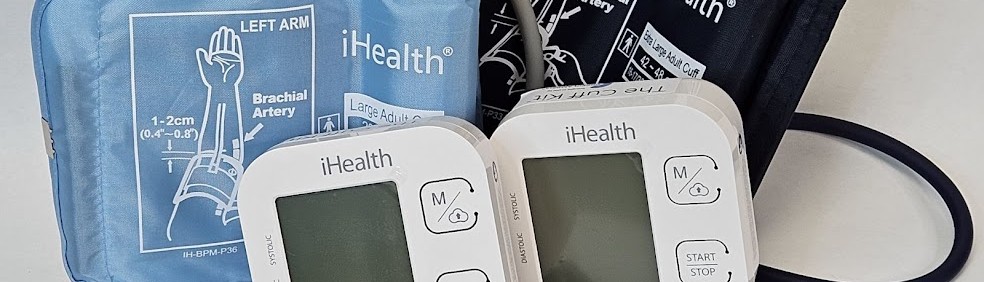
Congratulations on receiving your brand new Cuff Kit®! Want to learn more about how to use your iHealth Track device? Here are some handy videos and links to get you started. Unpacking and using...

Nurses play a vital role in detecting preeclampsia and caring for patient before, during, and beyond pregnancy.

A key component needed in the fight against preeclampsia is the development of tests for simple, rapid, and accurate diagnosis and prediction through the development and adoption of biomarkers.

Preeclampsia can strike quickly. Give new and expectant moms the best tool for early detection of hypertensive disorders with the Preeclampsia Foundation Cuff Kit® - a pregnancy-validated monitor wit...

Every woman should be able to check her own blood pressure at home.

Preventing and managing high blood pressure with healthy lifestyle behaviors are at the center of updated clinical guidelines published this week in the American Heart Association (AHA) peer-reviewed...

Hypertensive disorders of pregnancy are a leading cause of maternal death in the state of Indiana. To address this critical issue, the Indiana Hospital Association is teaming up with the Preeclampsia...

Recientemente, me encontré con una publicación en las redes sociales señalando la crisis de salud maternal desde la perspectiva de una mujer negra. Una persona respondió a...

For more on the Preeclampsia Foundation's work to amplify all research related to biomarkers for improved prediction and diagnostic tools, please visit https://preeclampsia.org/biomarkers. INDIANAPOL...

GAP—SPIRIN campaign gets low-dose aspirin to those most at risk to help close the maternal health gap in preeclampsia ________ NEW YORK, January 23, 2025/PRNewswire/ – In recognition of...
