
postpartum care
Delivery is not the cure for preeclampsia
Last Updated on December 30, 2024
Rethinking Postpartum Care for Patients at-risk for Hypertensive Disorders of Pregnancy
Women Need to Know they are Still at Risk after Their Baby is Born
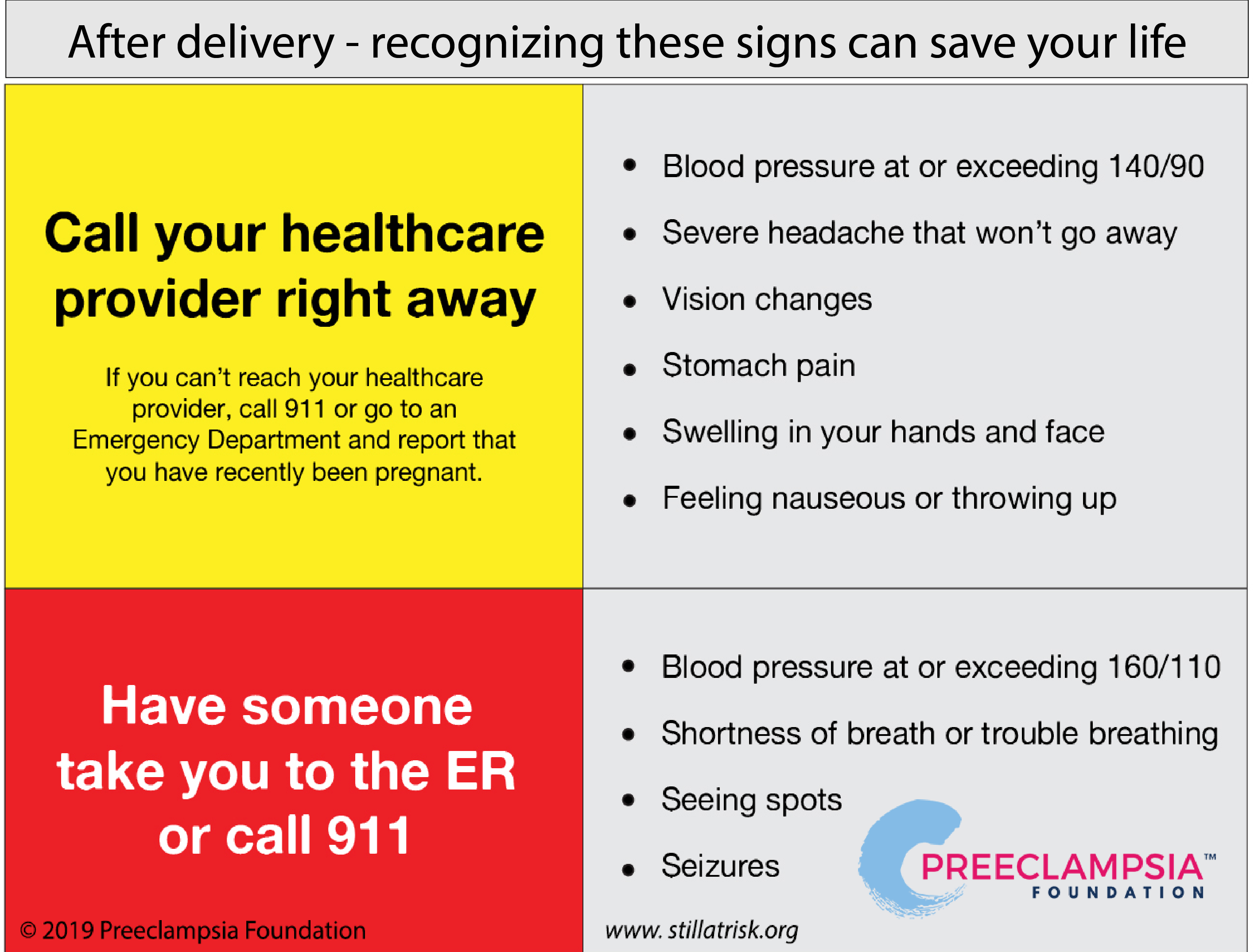
With 75% of preeclampisa related deaths happening after birth, the Preeclampsia Foundation has worked hard to debunk the myth that delivery is the cure for preeclampsia. We urge healthcare providers to educate their patients about postpartum preeclampsia and ask them to remain vigilant to any symptoms post-delivery. Any woman can develop preeclampsia after her baby is born, whether she experienced high blood pressure during her pregnancy or not.
Providers can order our postpartum tear pad here.
This guidance provided in “Postpartum Care Basics for Maternal Safety from Birth to the Comprehensive Postpartum Visit” is important for women who experienced preeclampsia or other hypertensive disorders of pregnancy for two major reasons:
- Many cases of postpartum preeclampsia are missed or poorly handled. Sometimes high blood pressure continues and causes other problems such as excessive fluid in the lungs or stroke. In other cases, new-onset high blood pressure – what is called de novo hypertension in medical terms – surprises some women after they’ve gone home, up to several weeks after delivery.
- The handoff from childbirth to a regular medical home must include transferring information about any pregnancy complications she experienced. Most women and even their healthcare providers are not aware that a history of severe preeclampsia, growth-restricted babies, and other pregnancy complications put them at higher risk for heart disease and stroke than other women without these complications. Your ongoing care should be managed through this lens.
“If a woman comes into my office and tells me she’s a smoker, I know she’s at higher risk for heart disease and we talk about what behaviors she can modify to reduce her risk. If a preeclampsia survivor comes into my office, I can’t change her pregnancy history, but we can work with her other modifiable risk factors and make sure we’re monitoring her heart health carefully,” explained Sue Kendig, a women’s health nurse practitioner and co-chair of ACOG's postpartum care bundle task force.
This postpartum care bundle suggests several items a healthcare provider should discuss with her patient while the woman is still pregnant and during the immediate postpartum period, planning for issues like breastfeeding, contraception, who will provide her medical care, and social support in the weeks following birth. It also states that every clinical setting must determine guidelines for patient education and indications for early postpartum visits such as coming in for another blood pressure check within four to seven days after delivery.
Make sure women know when and where to report symptoms. It is important if she shows up to the emergency department with high blood pressure that they understand she has been recently pregnant. This is something providers can help relay to their patients. More information for patients can be found at www.stillatrisk.org
Postpartum care and patient education remain a key goal for the Preeclampsia Foundation. Many of our affected women complain about the lack of information sent home with them, leaving them vulnerable when symptoms arise that should drive them back to care, but instead are ignored.
What is a patient safety bundle?
Standardization of healthcare processes and reduced variation has been shown to improve outcomes and quality of care. Patient safety bundles help facilitate the standardization process and reflect the latest clinical, scientific, and patient safety advances. The information should not be construed as dictating an exclusive course of treatment or procedure to be followed. Although the components of a particular bundle may be adapted to local resources, standardization within an institution is strongly encouraged.

Related Articles
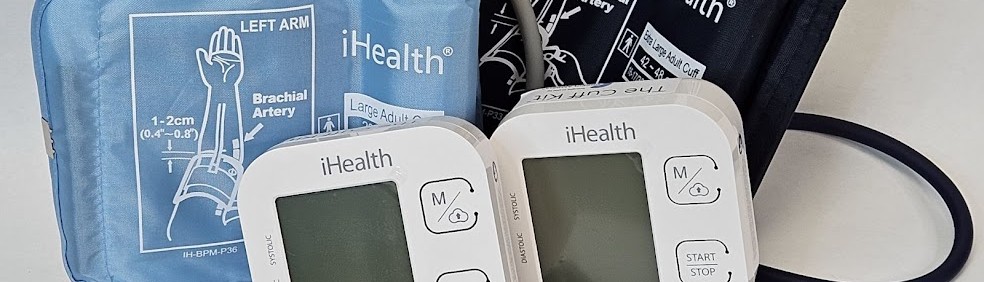
Congratulations on receiving your brand new Cuff Kit®! Want to learn more about how to use your iHealth Track device? Here are some handy videos and links to get you started. Unpacking and using...

Nurses play a vital role in detecting preeclampsia and caring for patient before, during, and beyond pregnancy.

A key component needed in the fight against preeclampsia is the development of tests for simple, rapid, and accurate diagnosis and prediction through the development and adoption of biomarkers.

As a first step to address the need for self-monitored blood pressure, the Preeclampsia Foundation started providing the Cuff Kit® in June 2020 to women at highest risk of developing preeclampsia and...

Every woman should be able to check her own blood pressure at home.

For more on the Preeclampsia Foundation's work to amplify all research related to biomarkers for improved prediction and diagnostic tools, please visit https://preeclampsia.org/biomarkers. INDIANAPOL...

GAP—SPIRIN campaign gets low-dose aspirin to those most at risk to help close the maternal health gap in preeclampsia ________ NEW YORK, January 23, 2025/PRNewswire/ – In recognition of...
1732072344.png)
While the Preeclampsia Foundation has been championing patient advocacy and representation for all families affected by hypertension in pregnancy throughout our 25 year history, we recognized the uniq...

Washington, DC – April 11, 2024 – On April 10, one day before the start of Black Maternal Health Week, the Preeclampsia Foundation in partnership with Thermo Fisher Diagnostics held a Hill...

Recently, I came across a social media post calling attention to the global maternal health crisis from a Black woman’s perspective. Someone responded to the post asking, “What’s rac...


